Review Article
Apexogenesis Therapies on Immature Permanent Teeth: Summary
401
Views & Citations10
Likes & Shares
The immature permanent tooth is a tooth who’s apical cemento-dentinal junction is not formed yet. Those teeth erupt before completing their root formation. They are characterized by enamel and dentinal structural immaturity with an open apex, short roots with thin and divergent walls. These particularities make the tooth more vulnerable to carious lesions and trauma, and therefore very singular to treat. Affected at an early stage, and when the immature permanent tooth is still alive, the objective of the treatment is to preserve this pulp vitality and to ensure the continuity of the physiological root formation.
In this work, we will explain the different apexogenesis therapies that can be performed on immature permanent teeth, in order to preserve pulp vitality and thus complete root formation. These therapies will be illustrated by clinical cases.
Keywords: Apexogenesis, Immature permanent teeth, Vital pulp therapy
Abbreviations: IPT: Immature Permanent Teeth; VPT: Vital Pulp Therapy; AAE: American Association of Endodontists; NaOCl: Sodium Hypochlorite; GIC: Glass Ionomer Cement; RMGIC: Resin Modified Glass Ionomer Cement; MTA: Mineral Trioxide Aggregate; Ca(OH)2: Calcium Hydroxide; CEM: Calcium Enriched Mixture; RNA: Ribonucleic Acid
INTRODUCTION
The immature permanent tooth (IPT), as its name suggests, is characterized by the immaturity of its structures:
-
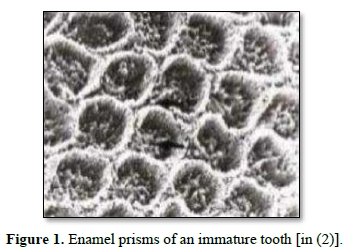
Enamel immaturity: Represented by surface irregularities formed by the perikymata which constitute an important porous network, in addition to its occlusal morphology that makes the tooth favorable to the retention of bacterial plaque [1] (Figure 1).
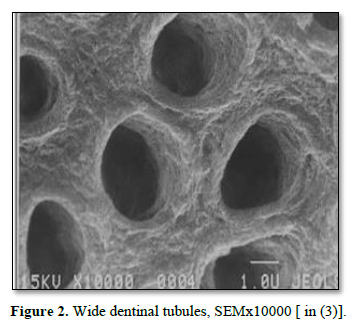
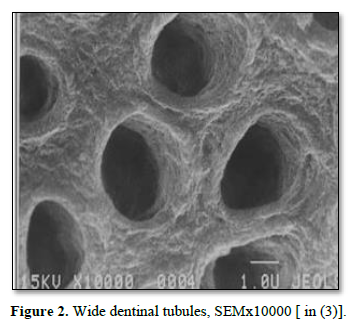
- Dentin immaturity: Represented by the absence of secondary dentin, which implies a large pulp volume without retraction of the walls of the chamber and the pulp horns. The peri-odontoblastic spaces are wide and invaded by tissue fluids, making the dentin more permeable [2] (Figure 2).
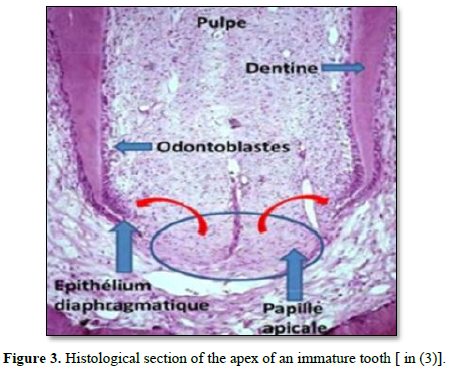
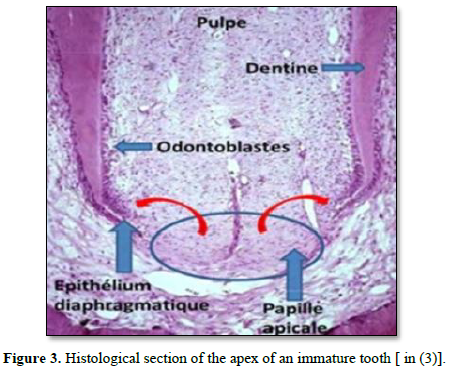
- Pulpo-radicular immaturity: The IPT is characterized by an apical region not fully formed, presenting an important vascularization and an intense cellular activity [3] (Figure 3).
This structural immaturity of the IPT makes it more vulnerable to carious and traumatic attacks, which is why we must consider conservative therapies (as long as the tooth is not necrotic yet). The main purpose of these therapies is to allow the tooth to continue its root development and preserve its vitality. We’re talking about apexogenesis therapies.
The American Dental Association recommends vital pulp therapy (VPT) for teeth with normal pulp or reversible pulpitis. The main idea of VPT is to avoid pulp exposure and long-term tooth retention, and consequently avoiding potentially painful, expensive and invasive root canal treatments [4].
Apexogenesis: According to the American Association of Endodontists (AAE), apexogenesis is defined as a vital pulp therapy that is performed to encourage continued physiological development of the root end [5].
- The apexogenesis pulp therapies of IPT are:
- Indirect pulp treatments
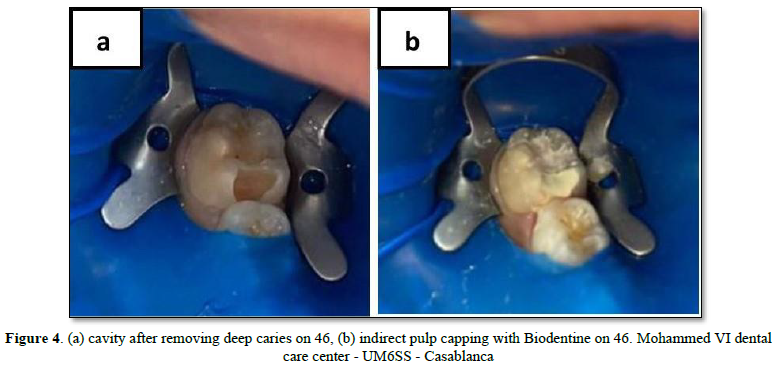
Indirect pulp treatment is a procedure in which a small amount of affected dentin is retained in deep areas of the cavity thereby avoiding pulp exposure. Then a material is placed on the affected dentin to stimulate and promote the recovery of the pulp [2]. This treatment is indicated in cases of vital pulp that presents a normal X-ray, without any history of irreversible pulpitis, and that does not require a major restoration or a complete crown [2,6]. There are two indirect treatment techniques: indirect pulp capping and the Step-wise technique. Indirect pulp capping is done in the same session, while the Step-wise technique requires a second intervention (Figure 4).
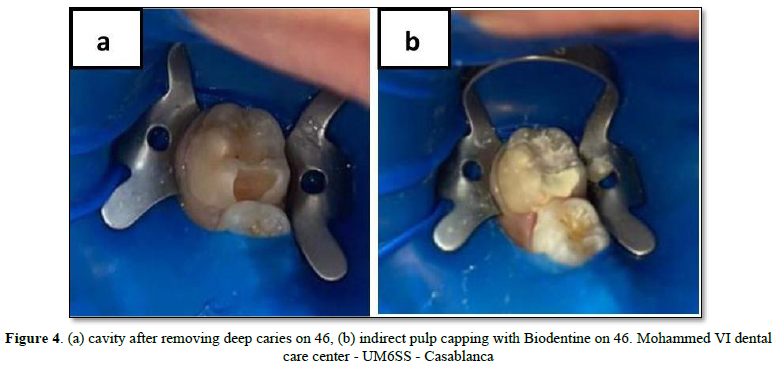
The indirect pulp capping procedure is as following: [2,6]
- Complete eviction of the infected dentine, and partial eviction of the affected dentine.
- Disinfection of the cavity with sodium hypochlorite (NaOCl) at 2.5% for at least 1 min.
- The placement of a capping material: Calcium hydroxide / Glass ionomer cement / Biodentine.
- The placement of a definitive well sealed coronary restoration.
According to a study by Reeves and Stanley, an affected dentin thickness of 1.1 mm after caries removal is a safe thickness where no pathological changes are noted. When this thickness is 0.5 mm or less, the formation of reparative dentin was observed and pulp pathologies (pulpitis and necrosis) were likely to occur. Therefore, indirect pulp capping has lower success rates since the inflammatory tissue is not totally removed, delaying the continuity of IPT radiculogenesis [7].
When pulp exposure is suspected, staged excavation of deep caries may be considered. This approach involves a two-step process. The first step is to remove the carious dentin along the enamel-dentin junction and excavate only the outermost infected dentin, leaving a carious mass above the pulp. The aim is to modify the cariogenic environment in order to decrease the number of bacteria, to isolate the remaining caries from the biofilm of the oral cavity and to slow down or stop the development of caries.
This temporary restoration must be able to be maintained for up to 12 months. The second step is the removal of remaining caries and placement of a permanent restoration [8].
The protocol of the Step-wise technique is as following (2 clinical steps): [2]
- Complete eviction of the infected dentine, and partial eviction of the affected dentine.
- Disinfection of the cavity with sodium hypochlorite (NaOCl) at 2.5% for at least 1 min.
- Placement of a temporary stratified restoration with: calcium hydroxide (CaOH2) + glass ionomer cement modified by the addition of resin (RMGIC) + Composite, or RMGIC + Composite. The material placed at the bottom of the cavity will be colored to facilitate its total elimination during the re-intervention.
- Re-intervention at 6 or 12 months to remove the restoration and the temporary cavity lining in order to check the remineralization of the affected dentin. Then a definitive well sealed coronary restoration will be carried out.
- Direct pulp capping
Direct pulp capping consists of the placement of a capping material on a pulp that has been exposed during the removal of the last layers of deep dental caries. The objective is to induce the formation of reparative dentin and preserve the pulp vitality of the IPT [2].
This pulp exposure should be minimal and punctual, not exceeding 1.5 mm. If it is a pulp exposure of traumatic origin, it should not go beyond 24 h [2].
Direct pulp capping can be performed on a vital tooth without signs of irreversible pulpitis or pathological radiographic signs, with controlled bleeding and limited coronal decay [2,6].
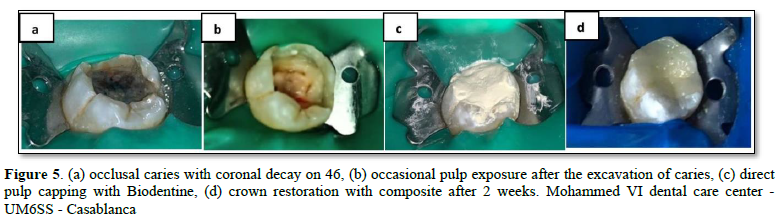
NaOCl is an effective hemostatic agent as well as a diagnostic tool to differentiate between reversible and irreversible pulpal inflammation. When the bleeding cannot be stopped after 10 min of direct exposure to NaOCl, there is a high probability that the coronary pulp is irreversibly inflamed and must be removed [4] (Figure 5).
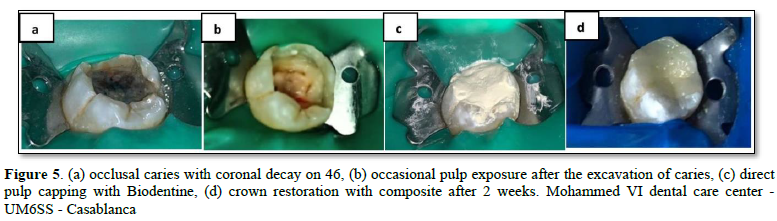
The protocol for direct pulp capping is as following: [2,6]
- Checking pulp vitality.
- Removal of the caries starting from the periphery to the depth.
- Cleansing the pulp wound with saline or NaOCl at 2.5% for 1 min.
- The placement of a capping material in contact with the wound (calcium hydroxide/ MTA/ Biodentine) without forcing.
- Cover the capping material with glass ionomer cement (GIC) and restore permanently.
- Partial pulpotomy
According to the American Association of Endodontists (AAE), it is the removal of a small portion of the vital coronal pulp as means of preserving the remaining coronal and radicular pulp tissues [5], which allows the continuation of radiculogenesis and the formation of a resistant tissue barrier.
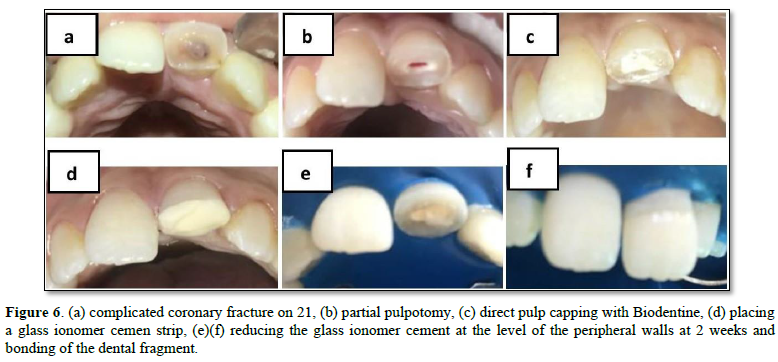
Partial pulpotomy is indicated in cases of carious or traumatic pulp exposure exceeding 24 h on a vital pulp, with controlled hemostasis and normal x-ray images [2,6].
Although the literature indicates that a Cvek pulpotomy (partial pulpotomy for traumatic pulp exposures) can be performed up to nine days after a pulp exposure, there is not enough evidence on the long-term outcomes of these teeth [8] (Figure 6).
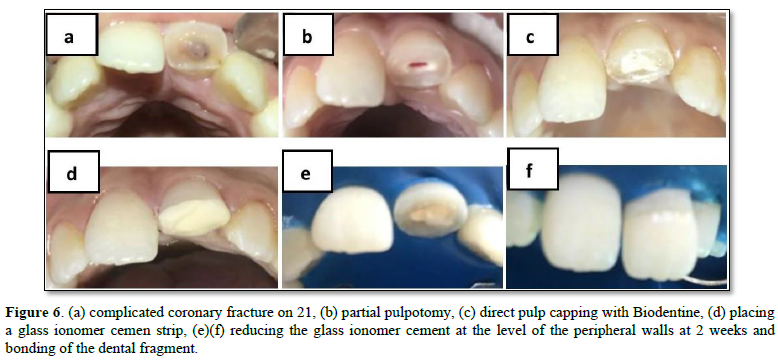
The partial pulpotomy protocol is as following: [2,6]
- Eviction of the carious tissue, then amputate 2 to 3 mm of the inflamed pulp with a diamond ball bur under irrigation.
- Apply pressure with a moist sterile cotton pellet to control hemostasis.
- Disinfection of the pulp wound and cavity with 2% chlorhexidine gluconate.
- Placement of MTA, Biodentine or calcium hydroxide on the pulp wound to a thickness of 2 to 3 mm.
- Placement of a sealed coronary restoration.
According to Uyar [9], the results of a randomized controlled trial on partial pulpotomy as a treatment for IPT whose pulp has been exposed by caries show that partial pulpotomy would be a valid alternative to apexification or conventional root canal treatment if the tooth has a diagnosis of normal pulp or reversible pulpitis [9].
Pulpal bleeding is controlled using irrigants such as sodium hypochlorite or chlorhexidine, then the site is covered with calcium hydroxide or MTA. MTA can cause dental dyschromia. Both versions of this material (clear and gray) have been shown to have similar properties. Although calcium hydroxide has demonstrated long-term efficacy, MTA allows for more predictable dentin bridge formation and pulp health [8].
- Cervical pulpotomy
According to the AAE, cervical pulpotomy consists of the elimination of the coronal portion of the vital pulp in order to preserve the vitality of the remaining radicular portion [5].
Complete pulpotomy of a vital immature permanent tooth aims to preserve the vitality of the remaining root pulp. The objective is to prevent undesirable clinical signs and symptoms, allow sufficient root development for endodontic treatment, prevent periradicular tissue degradation and avoid resorption defects or accelerated root canal calcification.
This will be analyzed in control sessions by periodic radiographic evaluation [8].
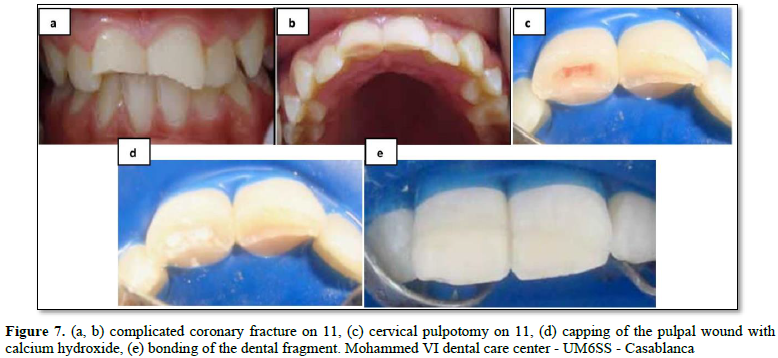
Its indications are identical to those of partial pulpotomy. The cervical pulpotomy will be done as a second intention if during the partial pulpotomy hemostasis is not possible [2,6] (Figure 7).
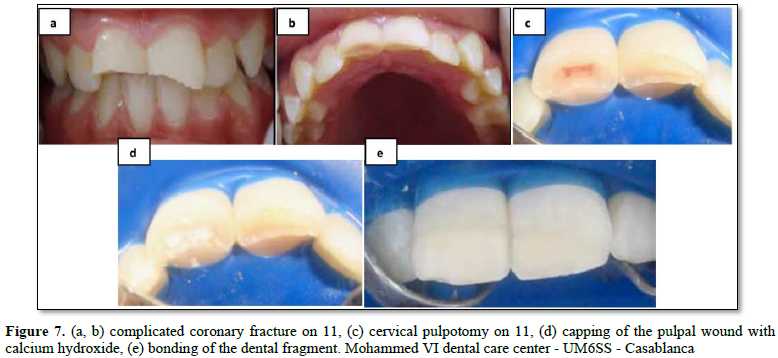
The protocol for cervical pulpotomy is as following: [2,6,10]
- Eviction of the decayed tissue and opening the access cavity.
- Amputation of all the cameral pulp, and ensuring hemostasis with a saline solution.
- Placement of a capping material: MTA or Biodentine or calcium hydroxide Ca (OH)2 to a thickness of 2 to 3 mm to cover the entire pulp stump.
- Placement of a sealed coronary restoration.
According to Chen [11], pulpotomy is an effective apexogenesis treatment to ensure the continuity of root edification on IPT with pulpal exposure. Therefore, a retrospective Cohort study by Shahmohammadi [12] reveals that cervical pulpotomy has the highest success rates compared to other life-saving pulp therapies.
For these different apexogenesis therapies, different materials are used, including MTA (Mineral Trioxide Aggregate), Biodentine, calcium hydroxide, or even calcium enriched mixture cement (CEM cement). Several studies have been carried out to compare the results obtained by each of these materials.
Uyar [9] showed that the results obtained with calcium hydroxide are poor, although this material was considered the gold standard for pulp capping. In fact, pulp capping with MTA had success rates of 96%, higher than when using calcium hydroxide.
The immature permanent tooth treated with Biodentine also had better clinical and radiographic results than calcium hydroxide. Biodentine induces the formation of a mineralized tissue which is thicker and less porous compared to that obtained by calcium hydroxide. Biodentine has become the alternative material for MTA since the latter has several disadvantages, such as longer setting time, setting expansion and dental dyschromia [9].
However, in a systematic review by Shenkin and Wilson [13], calcium hydroxide still retains its place as the pulp capping material of choice due to its antimicrobial properties and action in inducing reparative tissue. Furthermore, this material has some disadvantages such as the low modulus of elasticity and the high solubility in contact with water.
In another randomized clinical trial by Abuelniel [14] which compares MTA and Biodentine as materials used in pulpotomy of anterior IPT with trauma, the results showed that there is no significant difference between these two materials, except the appearance of dyschromia which is more prevalent in teeth treated with MTA (while those treated with Biodentine show color stability over time).
Recently marketed, CEM cement (calcium enriched mixture) is a new endodontic cement which has the same indications as MTA but has a completely different chemical composition [2].
This material (CEM) is obtained by a powder-liquid mixture. The liquid is in the form of a saline solution and the powder is essentially composed of: calcium oxide CaO, sulfur trioxide SO3, phosphorus pentoxide P2O5, and silica SiO2. The paste obtained is more fluid than that of MTA. The mixture is brought into contact with the dental organ in smaller quantities than the MTA, a thickness of 2ml is sufficient [2].
According to Chen [11], CEM cement has similar success rates to MTA and calcium hydroxide as capping materials in pulpotomy on IPT. Indeed, there is insufficient evidence that could draw a conclusion on the best material to use.
The success of apexogenesis treatments could be related to different factors such as the use of magnification (optical aids), antimicrobial washing of the cavity and wound, the capping material etc. But the most important success factor is the inflammatory state of the pulp [15].
Undoubtedly, the development of robust inflammatory biomarkers or other biomarkers, which accurately reflect the level of inflammation in the pulp, offers hope for objective measures of pulp inflammation while preserving pulp vitality, maintaining the integrity of the tooth and guiding the choice of treatment [15].
On the other hand, the capping material should evolve to target biological processes such as specific micro RNAs, epigenetic processes, antioxidants or by direct application of growth factors, which could result in the promotion of better-quality regenerative responses rather than reparative ones in the dentin-pulp complex, and consequently improving short-term scientific outcomes and potentially long-term patient outcomes [15].
CONCLUSION
The immature permanent tooth, in the years following its eruption, presents an immaturity of all the tissues which makes it vulnerable, in particular of the progression of caries.
It is essential to implement primary and secondary prevention strategies during this period. When more invasive therapies are necessary, it is essential to adopt them to preserve tissue and cell potential as much as possible, while adapting the treatment to the clinical situation that arises.
CONFLICT OF INTEREST
There is no conflict of interest.
- Vital SO (2012) Formation et physiologie de la dent pemanente immature: les répercussions cliniques Information dentaire. Réalités cliniques 4: 253-259.
- Simon L, Aucler C (2013) Le traitement pulpaire des dents permanentes immatures, thesis work, Nice Sophia Antipolis University Faculty of Dental Surgery.
- Zalane MI (2017) Apport du plasma riche en plaquette et plasma riche en fibrine dans le traitement des dents permanentes immatures nécrosées', thesis work, Abou Bekr Belkaid-Tlemcen University, Department of Dentistry.
- Doumani M, Arnous WA, Alsafadi MF, Alnazer HA, Alanazi SM, et al. (2020) The vital pulp therapy of permanent teeth: A dental practitioner's perspective from Saudi Arabia. J Int Soc Prev Community Dent 10(3): 300-308.
- Ave NS (2020) Glossary of Endodontic Terms.
- Cohenca N, Paranjpe A, Berg J (2023) Vital Pulp Therapy. Tooth Clin North Am 57(1): 59-73.
- Wu J, Li X, Xu L, Tang Z, Zhao J, et al. (2021) Radiographic evaluation of immature traumatized incisors following different endodontic treatments. Dent Traumatol 37(2): 330-337.
- American Academy of Pediatric Dentistry (2020) Pulp therapy for primary and immature permanent teeth. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry pp: 415-423.
- Uyar DS, Alacam A (2021) Evaluation of partial pulpotomy treatment in cariously exposed immature permanent molars: Randomized controlled trial. Niger J Clin Pract 24(10): 1511-1519.
- Bousfiha B, Elmouatarif F, Hejjouji K, Chliyah A, Elarabi S (2017) Réhabilitation esthétique par collage de fragment dentaire: Rapport de cas. Courrier du dentiste.
- Chen Y, Chen X, Zhang Y, Zhou F, Deng J, et al. (2019) Materials for pulpotomy in immature permanent teeth: A systematic review and meta-analysis. BMC Oral Health 19: 227.
- Shahmohammadi R, Sheikhnezami M, Moradi S, Jafarzadeh H, Azarpazhooh A (2021) Treatment Outcomes of Permanent Immature Teeth with Crown Fracture: A Retrospective Cohort Study. J Endod 47(11): 1715-1723.
- Shenkin J, Wilson L (2019) Mineral Trioxide Aggregate May Be the Most Effective Direct Pulp Capping Material. J Evid Based Tooth Practice 19(2): 183-185.
- Abuelniel GM, Duggal MS, Kabel N (2020) A comparison of MTA and Biodentine as medicaments for pulpotomy in traumatized anterior immature permanent teeth: A randomized clinical trial. Dent Traumatol 4: 400-410.
- Duncan HF (2022) Present status and future directions-Vital pulp treatment and pulp preservation strategies. Int Endod J 3: 497-511.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Advance Research on Alzheimers and Parkinsons Disease
- BioMed Research Journal (ISSN:2578-8892)
- International Journal of Diabetes (ISSN: 2644-3031)